does blue cross blue shield louisiana cover weight loss surgery
Anthem which operates Blue Cross and Blue Shield plans in 14 states Wednesday said net income doubled to nearly 23 billion in the second quarter ended June 30 compared to 11 billion in the. Body Mass Index BMI of 40 or greater OR.

Cigna Requirements For Weight Loss Surgery
Will follow two types of drug coverage.

. W8MDs insurance physician weight loss program is unique in many ways with a comprehensive multidisciplinary approach to weight loss that addresses all the complex issues leading to weight gain both in adults and children. Patients must be overweight and there must be a medical reason for the weight loss. BMI 35 399 AND one of the following.
In order to be pre-approved for the procedure you must meet the following requirements. A BMI of 35 or greater with at least 2 comorbidities. Examples of medical conditions that may be helped by weight loss include.
High blood pressure high cholesterol type 2 diabetes heart disease sleep apnea osteoarthritis and depression. Exceptions to the age requirement can be made for patients under 18 years old if a. If weight loss surgery is a covered benefit there is typically a section dedicated to the exact coverages for bariatric surgery and obesity treatment.
Blue Cross Blue Shield of Texas Criteria for Insurance Coverage. This page explains the coverage requirements plan types and covered procedures as. Leading insurance providers such as Blue Cross Blue Shield cover plastic surgery procedures when these are performed as a medical necessity and not for cosmetic reasons.
We get this question from most of our patients does blue cross blue shield cover weight loss surgery. How long does it take to get. I hear that bcbs of la.
1 and Trade names are the intellectual property of their respective owners. Blue Cross Blue Shield of Texas BCBSTX covers weight loss surgery. Are at least 80 lbs 36 kg overweight.
OUR BIGGEST LOSER LOST. Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies. You need must be between the ages of 18 and 60 years old.
Are between 18 and 75 years old. Have a history of failed weight loss attempts eg failed diets Thoroughly understand that the procedure is just a tool. And Southern National Life Insurance Company Inc comply with applicable federal civil rights laws and do not exclude people or treat them differently on the.
September 2016 Page 3 supportive treatment. A Body Mass Index BMI greater than 40. Blue Cross and Blue Shield of North Carolina is an independent licensee of the Blue Cross and Blue Shield Association Last Revision Date.
Alternatively you may qualify if your breast size causes significant symptoms such as. External links open in new windows to websites Blue Cross and Blue Shield of Louisiana does not control. These are the two most popular weight loss surgeries available and are both proven effective procedures.
A Body Mass Index BMI greater than 40. Blue Cross Blue Shield will then typically cover the cost of the surgery and the associated rehabilitation and. Blue Cross Blue Shield will cover weight management as long as the patient has a medical condition that is likely to be helped by weight management.
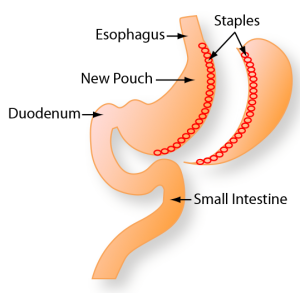
Florida Blue covers several bariatric procedures including the gastric sleeve or sleeve gastrectomy and the gastric bypass. Often youll be eligible for Blue Cross Blue Shield breast reduction coverage if your surgeon plans to remove at least 500 grams of breast tissue per breast. In order to be approved by Horizon Blue Cross Blue Shield of New Jersey for bariatric surgery in the United States you must meet the following criteria.
I am Okay with a waiting period up to a year if necessary. And SM Marks of the Blue Cross and Blue Shield Association. Primary Care Physicians Letter.
Your Anthem Blue Cross insurance policy covers weight loss surgery unless it states specifically that it excludes it. Blue Cross and Blue Shield of Louisiana and HMO Louisiana Inc. Yes insurance will cover skin removal after weight loss surgery when certain conditions are fulfilled.
If you are wondering does insurance cover skin removal surgery here. Be age 18 years of age or older. In order to be approved by Excellus Blue Cross Blue Shield for bariatric surgery in the United States you must meet the following criteria.
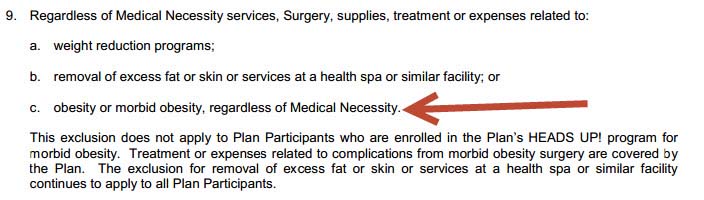
Weight loss coverage of various Blue Cross Blue Shield plans - an experience by a weight loss doctor. However some policies do specifically exclude weight loss surgery. Blue Cross and Blue Shield of Louisiana and its subsidiaries HMO Louisiana Inc.
Arkansas Blue Cross Blue Shield covers 5 weight loss procedures including the Gastric Sleeve Gastric Bypass and Duodenal Switch assuming your policy includes bariatric surgery. 3 Blue Distinction Centers for Bariatric Surgery Program Selection Criteria Cost Nationally consistent and objective approach for selecting BDC was used to address market and consumer demand for cost savings and affordable healthcare. Our patients are very afraid of these surgery fees but this varies from person to person and varies according to the fat ratio.
Each time the weight comes back do. The items below are the minimum necessary for approval of your weight loss surgery. 18 years of age special consideration if under.
Each anthem blue cross and blue shield california insurance policy can vary on what weight management or bariatric and gastric surgery expenses are covered or. Be Age 18 of age or older. Diagnosis of Morbid obesity defined as.
I am currently 35 bmi with apnea hi bp Hienal hernia and have tried every diet imaginable. Active Participation and Documentation of non-surgical methods of weight loss. I am looking for the right insurance plan to include Lapband surgery.
Long-term neck shoulder or neck pain. Use the contact information at the bottom of this page to find out if your policy has a specific exclusion for weight loss surgery. Some patients will be candidates for Lap-Band surgery which may also be covered by insurance.
The reason why we did not do this is to look at the weight loss rate of our patients. Long-term success requires significant diet and lifestyle changes. 2022 Open Drug Lists.
W8MDs biweekly program cost of 5000 covers up to two diet medications if dispensed in office. Patients who qualify for bariatric surgery usually. Thats typically determined by a doctor or a medical professional.
Diagnosis of Morbid obesity defined as. Grooving where the bra straps sit on the shoulder.

Bariatric Surgery Coverage Requirements Listed By Insurance Company

Weight Loss Surgery In Florida Grants For Medical
Gastric Sleeve Costs And Insurance Guide Bariatric Journal

Weight Loss Surgery In Florida Grants For Medical

Bcbs Of Alabama Weight Loss Surgery How To Avoid A Denial Bariatric Surgery Source

Medicaid S Criteria For Weight Loss Surgery

Bariatric Surgeries Now Covered By Insurance For Louisiana State Employees

Bariatric Surgery Coverage Requirements Listed By Insurance Company

Elipse Gastric Balloon Swallowable Nonsurgical Weight Loss Treatment Bariatric Journal
Weight Loss Surgery Extremely Beneficial Often Not Covered Wwltv Com
Bcbs Louisianna Hmo Coverage For Weight Loss Surgery
Medicare Coverage For Bariatric Weight Loss Surgeries Medicarefaq
/https%3A%2F%2Fd1l9wtg77iuzz5.cloudfront.net%2Fassets%2F2406%2F258949%2Foriginal.jpg%3F1551474667)
Low Cost Bariatric Surgery Affordable Weight Loss Solutions In Tijuana

Bcbs Louisianna Hmo Coverage For Weight Loss Surgery

Weight Loss Surgery Cost Georgia Bariatric Surgery Live Healthy Md

Don T Eat That Foods To Avoid After Bariatric Surgery

Elipse Gastric Balloon Swallowable Nonsurgical Weight Loss Treatment Bariatric Journal
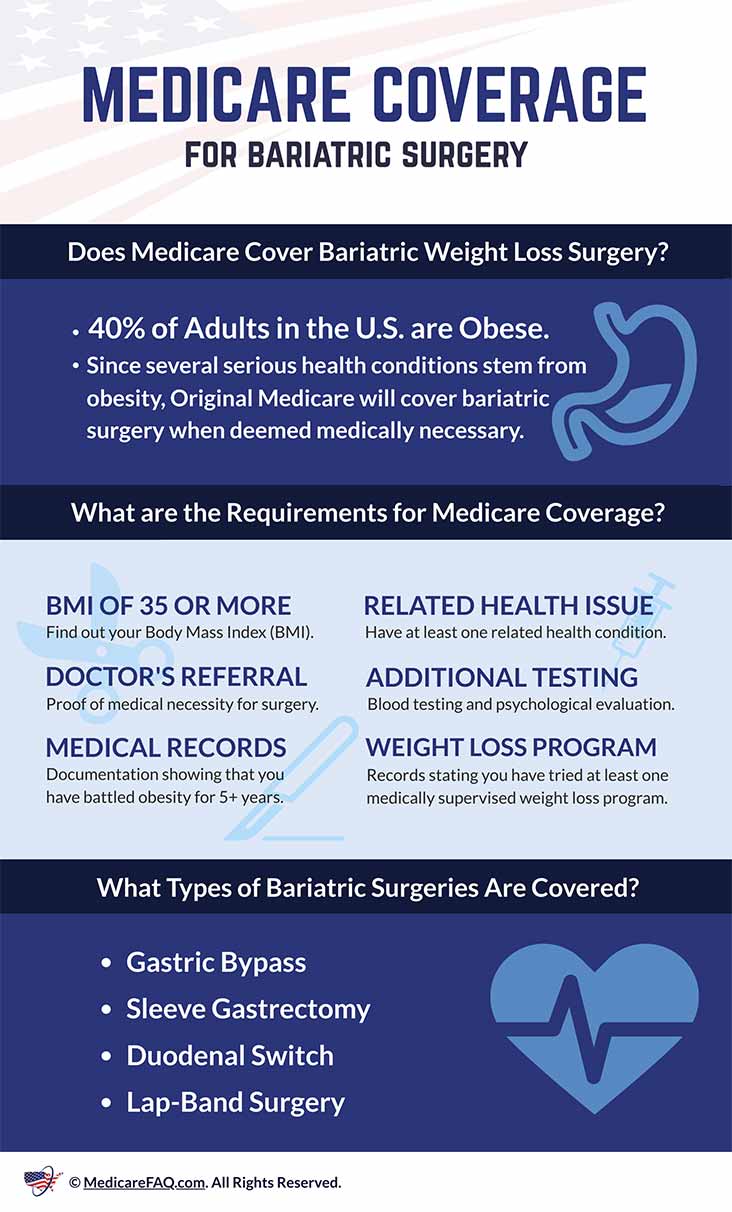
Medicare Coverage For Bariatric Weight Loss Surgeries Medicarefaq
